28 Mar 2014
Preventing Faulty Knee Mechanics in Gymnastics
Lauren Downes MSPT
Knee Anatomy
Injury prevention is a hot topic in gymnastics, as well as in many other sports. The forces placed on the body are very high in the spine, upper, and lower extremities. The knee joint, in particular, is very susceptible to injury due to the heavy load placed upon it. As a primary weight bearing joint, in addition to the patellofemoral joint, the knee is constructed of ligaments, meniscal cartilage, plica, and muscle tendons that can cause an athlete to experience pain. Knee injuries can present as a tear, muscle strain, dislocation, or referred patellar pain, and can limit or cease a gymnast’s ability to train.
There are several ligaments that create stability in the knee joint (See figure #1). The most commonly known ligament is the anterior cruciate, or ACL, and acts as the primary stabilizer of the knee. It attaches the tibia to the femur bone, and in conjunction with the hamstring muscle, prevents hyperextension of the knee. The posterior cruciate, which is not commonly injured, connects the same two bones and prevents hyperflexion of the knee joint. The two ligaments work together to provide a stable base for the knee during straight plane movements, as well as during rotatory forces. The lateral and medial collateral ligaments (MCL and PCL) are located on either side of the knee and connect the tibia to the femur medially, and the fibula to the femur laterally. These tissues help to prevent excessively valgus and varus stress on the knee. An often overlooked ligament is the medial patellofemoral ligament (MPFL), which connects the patella (kneecap) to the femur on the medial side, as well as part of the MCL. An athlete with instability in the patella is prone to injuring or tearing this ligament. (see figure #2).
Fig #1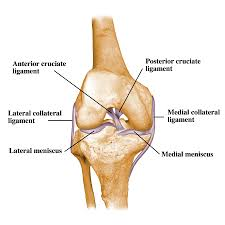 Fig #2 Fig #2 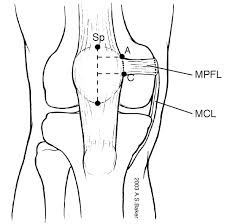
The medial and lateral meniscus (see figure #1) are the primary structures or cartilaginous tissue that act as shock absorbers in the knee joint, and act as a cradle on which the femur rolls and slides on the tibia bone. These small structures bear a great amount of weight and are susceptible to tearing with high impact and rotatory forces on the knee.
The second joint of the knee is the patellofemoral joint (see figure# 3). The patella is a small, odd shaped bone the sits on top of the femur. With flexion and extension of the knee, it glides in a groove that is located on top of the femur and tibia. The underside of the patella is shaped like a wedge, and when aligned perfectly, fits congruently in the groove when it slides up and down with movement. Patellofemoral pain syndrome (PFS) occurs when the patellar tracking motion deviates from the groove, causing the underside of the patella to rub on the femur bone. This condition is most common in teenage athletes, particularly females involved in a sport that involves high compressive forces on the knee joint.
Fig #3 Fig #4 Fig #4 
There are several muscles that control movement of the knee joint (see figure #4). The quadriceps muscle is a large group of muscles that span the front of the thigh from the hip to the knee joint. Above the patella it becomes the quadriceps tendon, which attaches to the patella. The patella acts as a fulcrum between the quad tendon and the patellar tendon, which crosses the knee joint and connects to the tibia. The primary function of the quadriceps is to actively extend the knee and to eccentrically slow down bending of the knee. The hamstring muscle group consists of three separate muscles that span the posterior thigh from the buttocks to the posterior knee. It actively flexes the knee and also helps to control hyperextension of the knee. The quadriceps and hamstrings are the primary movement controllers of the knee joint, in addition to several secondary muscles. The gastrocnemius (calf) muscle begins behind the knee joint and travels to the ankle, assisting in knee flexion. On the medial side of the knee, the adductor and sartorius muscles insert, but they act as primary adductors of the hip joint. The iliotibial band attaches to the lateral retinaculum of the knee, which is a fibrous tissue connect the patella to part of the quadriceps and the femur bone.
Lower Extremity Biomechanics
The structures of the knee, in a healthy, strong athlete, are designed to be strong and supportive, and can withstand high forces and loads placed upon it. Unfortunately, not every athlete is lucky enough to possess the perfect lower extremity biomechanics to maintain a healthy knee. For a knee to function properly, an athlete needs the following:
1) Synergistic and strong muscular balance of the hamstrings and quadriceps
2) Balance in flexibility of the muscles in the entire lower extremity
3) Properly aligned patellar
4) Normal mechanics of the arch of the foot
5) Strong core and hip musculature
Issues with any or a combination of the above factors can lead to injury, and should be addressed as part of an athlete’s training routine.
Since the hamstrings and quadriceps are opposing muscles that move the knee in opposite directions, they should have a similar balance in strength to support the knee joint. Females typically have a 2:1 ratio of quadriceps to hamstring strength, and that quadriceps dominance can contribute to patellofemoral pain or make an athlete more susceptible to an ACL injury. Weakness in the hamstrings can lead to posterior knee instability, and the knee may be slower to react to a hyperextension force that causes an ACL injury. An imbalance in these muscles can also alter a gymnast’s lower extremity mechanics and cause excessive compression at the patellofemoral joint. A tight, dominant quad muscle can increase the compression on the patella in a loaded position. When completing a strength training program, functional hamstring exercises such as single leg dead lifts, eccentric hamstring curls with sliding discs, and single leg bridges on a medicine or physioball should be performed in addition to traditional quadriceps exercises such as lunges in various planes and squats. To further challenge these muscles, a gymnast can perform the standing exercises on a ½ foam roll, balance board, or dynadisc to add a balance component to the exercise.
Balance in flexibility of the lower extremity muscles is a key component to injury prevention. It is important to note that movement in the hips and ankles have a direct effect on the movement of the knee joint. The entire kinetic chain affects each joint. Stretching muscles that oppose each other on either side of a joint is important to keep the joint gliding appropriately in both directions. For example, a gymnast should maintain good flexibility in the psoas (hip flexor) muscle in the anterior hip, as well as in the hamstring in the posterior hip. This allows the hip joint to rotate symmetrically into flexion and extension. If the psoas is too tight, it may cause excessive curvature in the spine or contribute to knee hyperextension. The iliotibial band is also an important muscle to stretch, massage or foam roll. Due to its attachments on the lateral side of the knee and its relationship to patellar tracking, the iliotibial band can contribute to patellofemoral pain if tight. As previously mentioned, the IT Band inserts at the lateral retinaculum, which can pull the patella laterally out of the groove it glides through. In most cases of patellofemoral syndrome, a tight IT Band is a major cause of faulty mechanics.
Fig #5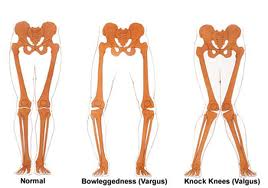
Other factors that contribute to abnormal patellar tracking, or an increase in the valgus angle of the knee (see figure #5), are foot pronation, weak hip musculature, and ligamentous instability. Some athletes are born with a hypermobile patella, which is caused by looseness in the retinaculum and MPFL. Unfortunately, ligaments cannot be tightened; therefore, it is necessary for an athlete to strengthen the muscles around the knee to compensate with muscular support. Foot pronation, or flat-footedness, is difficult to address in a gymnast, as a gymnast does not wear supportive footwear or arch support. When an athlete’s foot pronates, the arch drops towards the ground, and the tibia tends to rotate medially. This increases the valgus angle of the knee. You can see in figure #5 how this angle would affect the tracking of the patella. When you bend your knee, the hip and knee should line up over the foot. Any deviation from this position causes abnormal patellar tracking, which can cause patellofemoral pain or tendonitis. Since a gymnast cannot wear supportive footwear, he or she can experiment with arch taping methods, and consistently stretch the gastroc muscle, which can partially contribute to foot pronation.
The final topic to address is hip and core muscle strength, which is a key component to preventing knee injuries. Refer back to figure #5 and the valgus angle of the knee. In addition to excessive foot pronation, a weak glute medius can cause this position of the knee while bending. In a single leg squat, the glute medius muscle acts to stabilize the pelvis and hip. If it is weak, the opposite hip will drop, and the knee will begin to drift inwards. This movement pattern is very common in teenagers who are participating in sports at high levels, and is a major contributing factor in many knee injuries. Glute medius strengthening can be accomplished with both open and closed chain exercises. Open chain exercises include clamshells with an exercise band at various angles, and sidelying hip abduction with weights. The most effective closed chain exercises involve standing on one leg and working the leg in various planes of movement, such as a reach-pull exercise with a cable column or sport cord, lateral step downs, or single leg squats with a focus on pelvis stability. Core stability and strength also have a direct relationship to knee pain, as a gymnast needs to have a ‘stable base’ in the core musculature for other joints to function properly. If a gymnast has weak abdominals and lower back musculature, the entire kinetic chain of movement is affected. It is important to include core exercises in a training routine that involve stabilization of the trunk rather than repetitive abdominal crunch exercises. There are many training tools that will enhance a gymnast’s core training, such as sport cords, physioballs, medicine balls, and the TRX training system, to name a few.
In conclusion, it is imperative that a gymnast addresses all of the factors discussed to improve biomechanics and reduce risk of injury. This will reduce interruption of training and promote better health and wellness for the athlete.
|